The next time you’re in a doctor’s office…
and someone wraps a cuff around your arm to check your blood pressure, you’ll have to thank a nice Jewish doctor named Samuel Siegfried Karl Ritter von Basch. He called his device a sphygmomanometer, attempting to give it almost as long a name as he had. Dr. Von Basch was born in a ghetto in Prague and trained in Prague and Vienna. In the 1860s, he ended up chief surgeon in a military hospital in Mexico, actually volunteering for this assignment, if you can imagine that. I don’t think Mexican food was as tasty back then. Soon he was appointed personal physician to Maximilian I, a short-lived Emperor of Mexico put into power by the local nobility, with strong European ties who didn’t want the rank and file Mexicans running the country.
Maximilian I, uncle to Franz Ferdinand (of World War I assassination fame), was himself executed by Benito Juarez, Mexico’s future five-term president, who thought he needed to send a strong message to foreigners trying to take over his country. Maximilian’s physician, Dr. von Basch is best known in historical circles for his book Recollections of Mexico, which is a compelling firsthand account of the decline, fall, and execution of this short-lived Mexican Emperor. Recollections of Mexico, translated from the original German by one of Dr. von Basch’s relatives, with Amazon sales rank 2,166,150, is well respected among scholars of Mexican history. After the assassination, Dr. von Basch went to Europe and became an assistant professor at the University of Vienna, the same school that taught Albert Einstein and had Sigmund Freud on the faculty.
Physicians had long known that blood circulated around the body under pressure, but there was no noninvasive way to measure this pressure. When it was discovered that you could push on an artery and shut off the flow of blood (I would like to have received the Nobel Prize for that discovery), the search was on for a way to measure this occlusion pressure.
In 1881, Dr. von Ba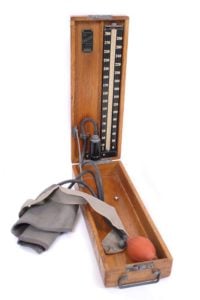
Others refined the invention by using the inflatable cuff we know today and hooking it to a column of mercury. By 1901 the sphygmomanometer was in widespread use, but we were still only measuring the top number, or systolic pressure. However, when you think about it, the heart pumps blood around the body in a pulsatile fashion. The flow is not like the flow of water in your kitchen sink, but instead is more like a repetitive jet squirting out, like a Waterpik, or like the flow of air when you pump up a bicycle tire. When the heart is refilling with blood in its relaxation phase, does the blood pressure in the body fall all the way to zero? Is the pressure in a bicycle tire zero between pumps? Surely not.
It fell to Nikolai Korotkov, a Russian vascular surgeon, to get us the second number, or diastolic blood pressure. This is the pressure in the arterial system during the relaxation phase before the heart contracts yet again. In a short note in a Russian military medical journal, he described listening with a stethoscope, instead of feeling the artery with one’s fingers. Korotkov identified a series of sounds that allows us to determine the diastolic pressure. Fact is, if you take a stethoscope and listen over a normal artery, you hear nothing. Although the blood flow is pulsatile, it flows fairly smoothly, but if you partially occlude the artery, you introduce turbulence, just like partly kinking a hose will produce a noisier flow of water. Korotkov figured out that at a sufficiently high cuff pressure, you hear nothing because there is no blood flow. As the pressure is let out of the cuff, some blood starts flowing, but only during that part of the heart cycle when the pressure rises high enough to get past the tight cuff. This makes a noisy, “whoosh, whoosh” sound. As the press
Sometimes, the doctor or nurse cannot hear anything when listening over the artery.
Rather than making up numbers, it is better to revert to the pre-Korotkovian era
and just feel when the artery starts pulsating as you let the pressure out of the cuff.
Sometimes, the doctor or nurse cannot hear anything when listening over the artery. Rather than making up a set of numbers, it is better to revert to the pre-Korotkovian era and just feel when the artery starts pulsating as you let the pressure out of the cuff. This only gives you the top or systolic blood pressure, but that is still helpful in many situations.
We can even take blood pressure in the ankle and compare it to the pressure in the arm. If the ankle pressure is much lower than the pressure in the arm, we conclude that there is a narrowing of the arteries during the long path to the ankle, as compared to the shorter path to the elbow.
You can buy an automated blood pressure monitor from the drugstore for $25. Here at MedNorthwest, we have a $1,500 automated blood pressure device. Maybe the sales guy knew we were a concierge medicine practice and added a zero to the invoice, but it is helpful to have a pretty accurate machine here, even if home blood pressures are a better reflection of true blood pressure, although less precise.
Unlike some diagnostic tests from the 19th century, such as phrenology, determining blood pressure has remained of great value up to the present and is a key diagnostic sign in internal medicine, cardiology, emergency medicine, and pretty much all of health care.