Vertigo means dizziness—actually a specific …
kind of dizziness where you think the room is spinning or moving, as opposed to feeling unsteady on your feet with reasonably stable surroundings.
Any child who has experimented with spinning around like a top knows the sensation of vertigo. My own introduction was at age four, when my mother played Harry Belafonte’s “Jump Down, Spin Around, Pick a Bale of Cotton” on her record player. The song’s lyrics encouraged me to do just that, and my mom was loving enough to throw cotton balls on the floor to enrich the experience. When Mr. Belefonte was done singing, I collapsed on our black leather sofa, and the room spun for about a minute. That was vertigo.
Linguists at the Department of Redundancy Deptartment. sometimes recommend the term true vertigo. Among physicians, this means not only is the patient complaining of the room spinning, but that the doctor actually took the time to have the patient distinguish between feeling unsteady or really sensing the room spinning.
 There are many different types of vertigo. The most common type I see in my practice is benign positional vertigo. In this context, benign has nothing to do with a tumor or growth; instead, it means that the cause is not serious. A serious cause of vertigo might be multiple sclerosis or a stroke. Positional means that the vertigo comes on with certain head positions; vertigo means the room is really spinning.
There are many different types of vertigo. The most common type I see in my practice is benign positional vertigo. In this context, benign has nothing to do with a tumor or growth; instead, it means that the cause is not serious. A serious cause of vertigo might be multiple sclerosis or a stroke. Positional means that the vertigo comes on with certain head positions; vertigo means the room is really spinning.
Benign positional vertigo, or BPV for short if you’re a cool neurologist, or BPPV (if you want to throw the word paroxysmal which means occurring at sudden, unexpected, intervals), is very common. A typical case starts out in the morning. A patient wake up, turns to look at the alarm clock, and the room starts spinning violently. He or she might get up and try to make it to the bathroom, but sometimes it can be nearly impossible to walk. Patients do not note any change in their hearing, and there is no numbness or weakness. If a patient holds still, the dizziness settles down, but as soon as the head is turned in a particular direction, the dizziness starts up again. By the time patients make it in to see me, they have usually figured out which type of head turning causes the most trouble. Also the symptoms are usually better, but not completely gone.
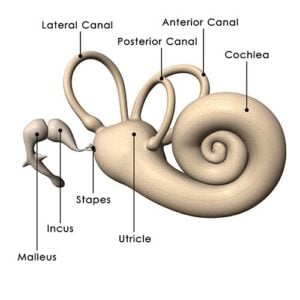
What’s going on here? Well, to understand BPV, we need to know how the body keeps its balance. One of the many mechanisms for balance is the three semicircular canals inside each of your ears. These are very similar to the canals in Venice, except that you can’t float down them in a gondola. Instead, each is oriented at about a right angle to the other. When your head turns, fluid in these canals, called endolymph, moves and causes little hairs at the base of the canals to move. This is one important way the body’s balance system detects movement. To appreciate how this system works, if you nod your head up and down and shake it side to side, you can still read this text, but if you move the paper around, it is very hard to keep on reading. The semicircular canals know when your head is moving and can keep your eyes fixed on an object even if you are running or riding on a bumpy road. If this system breaks down, when you walk along the street, the world seems to jump up and down- a phenomenon called oscillopsia.
Normally, a tiny rock of calcium, called an otolith, sits on top of each hair cell. (Oto = ear, lith = stone, as in lithotripsy or Mick Jagger and the Rolling Liths.) This weight makes the hair cells droop a bit from gravity and lets the body know which way is up or down without looking. With BPV, the symptoms are thought to occur when an otolith falls off the hair cell and enters the semicircular canal. Like an American in a powerboat entering the quiet canals of Venice, this causes a considerable disruption. Then, when you turn your head, the “rock” causes the fluid to shift more violently and this sends a false message of movement to the brain. Your eyes attempt to track this movement (just as they successfully did when you moved your head around while reading), but in reality, your head is not moving, so the room appears to spin. If you hold still, the rock doesn’t move and you feel better.
If you repeatedly move your head around and try to make yourself dizzy, the brain figures out that it is receiving a false signal and it begins to suppress the data from that ear. So one trick with BPV is this: Although you feel worse moving your head, if you keep moving, the dizziness will actually get better. In emergency medicine, I commonly saw patients who were worse at home and better when they came to the ER. Coming in produced a lot of head movement which reduced symptoms.
A treatment called the Epley maneuver purports to get the otolith out of the semicircular canal and fix the dizziness. I’m not sure how much of this maneuver is just moving a patient around enough to get the brain to shut off listening to that ear’s balance data, and how much of it really is getting a microscopic rock back out of the way. I generally recommend patients move their head in the direction that causes the most dizziness and do this several times to alleviate the dizziness.
Physicians use the Hallpike-Dix maneuver to diagnose BPV. Patients are taken from the sitting position to supine and then the head is tilted back, sometimes over the edge of the bed, and turned at about a 45-degree angle. After a few seconds, this causes rapid eye movements called nystagmus. With nystagmus, the eyes are trying to compensate for a turning head, but the head is not turning.
Another common cause of dizziness is labyrinthitis. This is presumed to be a viral infection causing inflammation of the entire inner ear. Because the entire inner ear is involved, there is also hearing loss. In vestibular neuronitis, just the nerve of balance is inflamed, but nothing else involving the inner ear, so hearing is preserved. In both of these conditions, the dizziness is more continuous and is not dramatically worse with certain head movements or positions over others. Medicines used to treat motion sickness can be helpful here along with vestibular rehabilitation. One study showed that high doses of prednisone help patients recover balance in vestibular neuronitis.
A treatment called the Epley maneuver purports
to get the otolith out of the semicircular canal
and fix the dizziness.
Patients experiencing dizziness often worry that it is a sign of stroke. With a stroke, dizziness is usually not the only symptom. Patients will generally also have double vision, trouble speaking, numbness, weakness, or other neurological symptoms. We distinguish central vertigo, vertigo arising in the brain from a stroke, multiple sclerosis, and so forth, from peripheral vertigo, vertigo arising from the ear. Obviously, central vertigo is more serious. If we suspect a central cause of vertigo, an MRI is very helpful in sorting things out. Central causes are more rare.
So if you wake up one morning, turn to look at the alarm clock, and the room starts suddenly spinning, you might have benign positional vertigo. If you have hearing loss and dizziness after a bad cold, you may have viral labyrinthitis. If you have double vision and are so dizzy you can’t walk and one half of your tongue is numb, well, that might be a stroke. Patients who are suddenly dizzy should come to see me. We can start with a simple work-up in the office and proceed to sophisticated studies such as an MRI, if necessary, based on the presenting symptoms.